Schedule Your Appointment
MAGNOLIA & WOODLANDS
(281) 789-3400
CYPRESS
(281) 503-8160

Click here if you saw our HAERT
Covid-19 Testing Information

Location & Hours of Operation
Dates and times subject to change.
- Appointments are required. Please click here to register.
- The testing calendar opens up for bookings 3 days in advanced at a time. If there are no appointments available within 3 days from today’s date please check back often as cancellations do occur which will open time slots back up.
- Testing is available for people who are symptomatic as well as asymptomatic
- Pre-screening or a doctor’s note are not required to get tested
- All ages can be tested
- Cash and credit cards accepted for self-pay
- Insurance will NO LONGER be billed for Covid Testing
Please note: Only two appointment are available every 15 minutes. Please schedule accordingly if you desired appointment slot is not available or if you have two or more people you wish to have tested. Please do not arrive before your scheduled appointment time. You may not be allowed entry until your appointment.
Testing Options
Testing is open to everyone regardless of what county you reside in.
PCR Swab Test
PCR testing is used to directly detect if COVID-19 is actively present in your system and will determine if you are contagious. If you have contracted COVID-19, it usually takes 3-7 days for you to have enough virus in your system for the test to show a positive result.
- Nasal swab
- Results in 3-5 days
- Self-pay PCR swab test: $200
- Cash and credit cards accepted
- Insurance will NO LONGER be billed
Appointments are required before you arrive.
Antigen Test
Antigen testing is a rapid, effective, and direct testing method for determining if you are contagious with COVID-19 within days after symptom onset or within a week of known exposure. If you get a positive result it is recommended to follow up with a PCR test to confirm the findings.
- Nasal swab
- Same day results
- Self-pay antigen test: $125
- Telehealth discussion with provider to go over results included
- Cash and credit cards accepted
- Insurance will NO LONGER be billed
Antibody Blood Test
The antibody blood test is used to determine if you were previously exposed to COVID-19 and have developed antibodies to the virus. It does not tell you if you have an active infection of the virus. It can take between 7-21 days to produce enough antibodies in your system to show a positive result.
- Tiny finger prick for blood sample
- Same day results
- Self-Pay antibody blood test: $75
- Telehealth discussion with provider to go over results included
- Cash and credit cards accepted
- Insurance accepted (Patients with Medicaid will be required to pay cash pay rates for all COVID-19 testing)
TEMPORARILY UNAVAILABLE
Testing FAQs
PCR Swab Test
Is your PCR swab test FDA approved?
We do not analyze PCR studies we only collect samples and then send them to the lab to be processed. Our specimen collection kit is approved by the CDC and our labs follow CDC guidelines for processing tests.
Do I need to have symptoms to be tested?
No. Studies are showing at least 50% of patients do not show symptoms even if they have COVID- 19. Anyone can be tested here if you feel you have been exposed or are at risk of exposure.
Does everyone in my family need to be tested?
If you live in close proximity to others in your family and test positive for COVID-19, you may have already passed the virus to them without even knowing it. Because of this, you do not need to test everyone in your family. However, if you feel the need to have all family members tested, they can be tested.
I just got screened and tested for COVID-19, what do I do now?
If you are symptomatic or believe you may have been exposed but are not showing symptoms, please quarantine yourself and family until you get your test results. Regardless of your symptoms or test-results, always follow any local “stay-at-home” or “shelter-in place” guidelines, monitor your employer’s restrictions on returning to work, and practice strict hygiene such as frequent hand washing, covering your mouth when you cough or sneeze, avoid sharing household items, and clean surfaces of your home regularly. Try to restrict all non-essential activities outside of your home. If you are in public areas be sure to practice social distancing and wear a mask.
What type of test did I receive, and will this test tell me if I am immune to COVID-19?
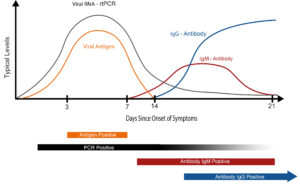
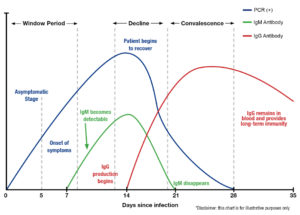
PCR swab tests are screening for the presence of the active COVID-19 virus in your system and do not test for antibodies which can provide you with immunity. However, there are tests that show if your body has been exposed to COVID-19 and has produced protective antibodies which may provide you with immunity to the virus. America’s ER is now offering rapid result antibody testing (10 minutes) that will show the presence of COVID-19 antibodies, specifically IgM and IgG, in your system. When used in conjunction with the PCR swab test, antibody testing is a powerful tool to tell if you were exposed to coronavirus, where you are in the disease spectrum, if you are still contagious, and if you have developed immunity antibodies to COVID-19. This test requires a small blood sample from a finger-stick similar to those seen with diabetic blood glucose monitoring.
Where do you send my test?
We have the capabilities to test in-house. Your tests are not sent out to a lab.
When will I receive my test results?
You will receive your results the same day you tested, in most cases, depending on the in-house case loads.
How will I be notified of my test results?
A staff member of America’s ER + Urgent Care will contact you via phone call and/or email.
What should I do if my test results are negative?
No test is perfect. In some cases, you may have taken the test before there was enough virus in your system to be picked up with testing, you are someone who received a false-negative test result (in other words, you are positive but the test didn’t pick up the virus), or even though you were sick, COVID-19 was not the cause of your illness. While PCR swab tests are the best way to tell if you are actively carrying COVID-19 and are contagious, a single negative test doesn’t mean you do not have the virus, especially if you have not had symptoms before getting tested. Only antibody blood testing done at about a week from contracting the virus will be able to tell if you have been exposed to COVID-19. Also remember, if your results are negative or are later exposed to someone with COVID-19, you may still be at risk of contracting the virus, developing symptoms, and require additional testing.
What should I do if my test results are positive?
Don’t worry. Patients are recovering from COVID-19 every day and most only experience mild flu-like symptoms. Always follow the instructions above regarding quarantining, personal hygiene, and restrictions in activity. If your test results are positive, we will report our findings to local health departments and other regulatory agencies. If additional information is needed, antibody testing is recommended, or confirmation testing is required, you will be notified at the number you provided.
Will I get a prescription for Hydroxychloroquine and Azithromycin if I am positive?
These medications are in high demand following news reports showing their effectiveness in combating the virus. However, the federal government is limiting those who are qualified to receive these medications. Even if we provide you with one, there is no guarantee your pharmacy will fill it.
When should I seek medical care or visit an emergency room?
Seek emergency care if your symptoms worsen or you are experiencing difficulty breathing, tightness in your chest, high fever, or any other alarming symptom. Before seeking care, call your healthcare provider and tell them you have been tested for COVID-19. Please wear a mask before entering any facility.
When can I return to work?
Please follow the most recent local, state, and federal guidelines regarding testing requirements for returning-to-work.
Rapid Same Day PCR Testing
Why should I get a rapid same-day PCR test?
Rapid same-day PCR testing is suggested for those requiring evidence of PCR testing for travel purposes or other reasons that are not considered medically necessary.
What is the cost of rapid same-day PCR testing?
The cost of rapid same-day PCR testing is $200 at the time of service. Payment can be made by cash or with credit card.
Does this test cover all variants of COVID-19, including Omicron?
The manufacturer of our rapid same-day COVID-19 PCR test, Cepheid (https://www.cepheid.com/coronavirus), reports it is capable of detecting the COVID-19 Omicron variant (SARS-CoV-2, B.1.1.529).
How soon will I get my results?
Depending on testing volume throughout the day, you can typically expect to receive your rapid same-day PCR results within a few hours of receiving your test. You will receive your results no later than 24 hours after taking your test.
How will I get my results?
Your test results will be emailed to the email you provided during registration. If you do not have access to an email address, you may visit one of our locations in person and request a print out of your results.
How soon should I get this test if I have travel plans within the next 72 hours?
Most major commercial airlines and cruises require you have a negative COVID-19 PCR test performed within 72 hours of travel. The rapid same-day COVID-19 PCR test is strongly recommended if you are traveling within the next 72 hours. If you choose not to obtain a rapid same-day COVID-19 PCR test at any of our locations or through our drive-through, we cannot guarantee delivery of your test results within the 72 hour timeframe and cannot be held responsible for any required changes in your travel plans due to delayed results.
Antigen Test
What is an antigen?
An antigen is a small molecule, often a protein with a distinct shape, our bodies see as foreign, and is capable of stimulating the body’s immune response. When exposed to these microscopic invaders, our immune system begins the process of protecting itself by binding antibodies to these antigens and neutralizes them or tags them for destruction by other cells. COVID-19 has several known antigens, with the most recognizable being its spike proteins, or coronas, from which the virus gets its name.
How do they work and why are they important?
Antigen testing is a rapid, effective, and direct testing method for determining if you are contagious with COVID-19 within days after symptom onset or within a week of known exposure. Antibody tests, in contrast, must wait 2-3 weeks after exposure for the body to develop an immune response to very specific COVID-19 antibodies. In other words, even though antibody test results are accurate and fairly immediate, antibody testing looks for the evidence of a previous infection as opposed to the virus itself. PCR tests on the other hand, while over 98% accurate and the only FDA approved test for diagnosing an active COVID-19 infection by detecting viral genetic material, require advanced labs and can take days to get results. In addition, PCR can be so sensitive, inactive viral RNA can also be detected weeks, and sometimes months following recovery resulting in multiple positive COVID-19 PCRs even though you are no longer contagious.
Antigen tests work by identifying specific proteins on a particular pathogen where known antibodies attach and then mimick that immune response artificially. If there is a successful match between the COVID-19 antigen and manufactured coronavirus antibodies, the test is “positive” and we know you are contagious with active virus. In addition to its relatively ease of interpretation through the use of automated analyzers, Antigen tests also have the benefit of quick turnaround times with results available in as little as 15 minutes.
What test does America’s ER use and is it FDA approved?
America’s ER utilizes Quidel’s Sophia SARS Antigen IFA test kits and analyzers (https://www.quidel.com/), a US-based rapid antigen test manufactured in California. Quidel was issued an emergency use authorization (EUA) from the FDA in late May 2020 after proving their tests delivered reliable and consistently accurate results for detecting COVID-19 antigens. Quidel is one of two Antigen tests trusted by the US government.
Do your tests test for every strain of COVID-19?
The Sofia SARS Antigen FIA test does not test for every strain of COVID-19 and therefore does not differentiate between SARS-CoV, SARS-CoV-2 or variants of SARS-CoV-2.
Are your Antigen tests accurate? What about “false-negatives” or “false-positives”?
Quidel reports 96.7% PPA (positive percent agreement) when compared to rt-PCR as recently as July 17th, 2020. Due to the very narrow window when these tests are positive (3-10 days after symptom onset), patients who receive the test outside of that window may experience what is known as a “false-negative,” meaning the received a negative result even though you still have viral genetic material in your system. “False-positives,” or test results demonstrating a positive result when you are negative is very unlikely with this testing platform given the manufacturer’s reported specificity and level of sensitivity.
Who should get an Antigen test and when should I get it?
Antigen testing should occur after 3 days of symptoms consistent with COVID-19. Alternatively, Antigen testing is an excellent method for asymptomatic patients 5-10 days from known COVID-19 exposure to determine if they contracted the virus and are now contagious. Antigen testing can also be used effectively as a rapid screening test for COVID-19 given the quick turn-around and relative accuracy.
You collected a specimen from my nose. Does that mean antigen tests and PCR tests are the same?
Antigen tests and PCR tests are not the same. The coronavirus lives and replicates in the upper respiratory tract and because both PCR and antigen tests are testing for active virus, specimens must be taken from that area and why you are swabbed with both. However, that is where their similarities end. PCR tests (more specifically rt-PCR), or reverse-transcriptase polymerase chain reaction, are taken to a lab where the RNA removed from the virus, coded into DNA, and then amplified so parts of COVID-19’s genome can be detected via advanced techniques. This is why it is so sensitive and considered the only FDA approved diagnostic test for COVID-19. Antigen tests, as discussed above, are comparatively simple and require less equipment to interpret. If you are required to obtain a PCR test, be sure to get a PCR test because they are not the same.
How and when do I get my results?
The Antigen test takes about 15-20 minutes to produce results. You will be called by one of our medical providers the same day that you take your test to go over results. Please note it may take several hours to receive your phone call due to the number of patients our providers are calling but you will receive a phone call the same day of your test.
If I test Positive will I need a follow-up PCR test?
Both America’s ER and Quidel, the Antigen test’s manufacturer, recommend all patients obtain a PCR swab test for confirmation of any findings.
Can I go back to work or school after getting this Antigen test? Will I get a doctor’s note?
Because Antigen tests are non-diagnostic according to the FDA, America’s ER cannot provide clearance to return to work or school. While we can provide scientifically supported opinions based on your test results as well as containment strategies and quarantine recommendations in the event you are Antigen positive, it is ultimately your employer’s and or school district’s responsibility to establish their own guidelines in light of existing local, state, and federal mandates imposed during the national emergency and to decide if you are free to return to work/school following testing. For your privacy and the protection of your health records, America’s ER does not release your medical records to any third party unless a release of medical records have been signed, is on file, and you have instructed us to forward specific portion(s) of your healthcare record.
With that said, when timed correctly, combining, PCR, Antigen, and Antibody testing can provide a very clear picture of your current infection status, if any, and risks of infecting others. Please refer to the CDC’s website for more information on testing strategies and return to work/school criteria for both symptomatic and asymptomatic patients.
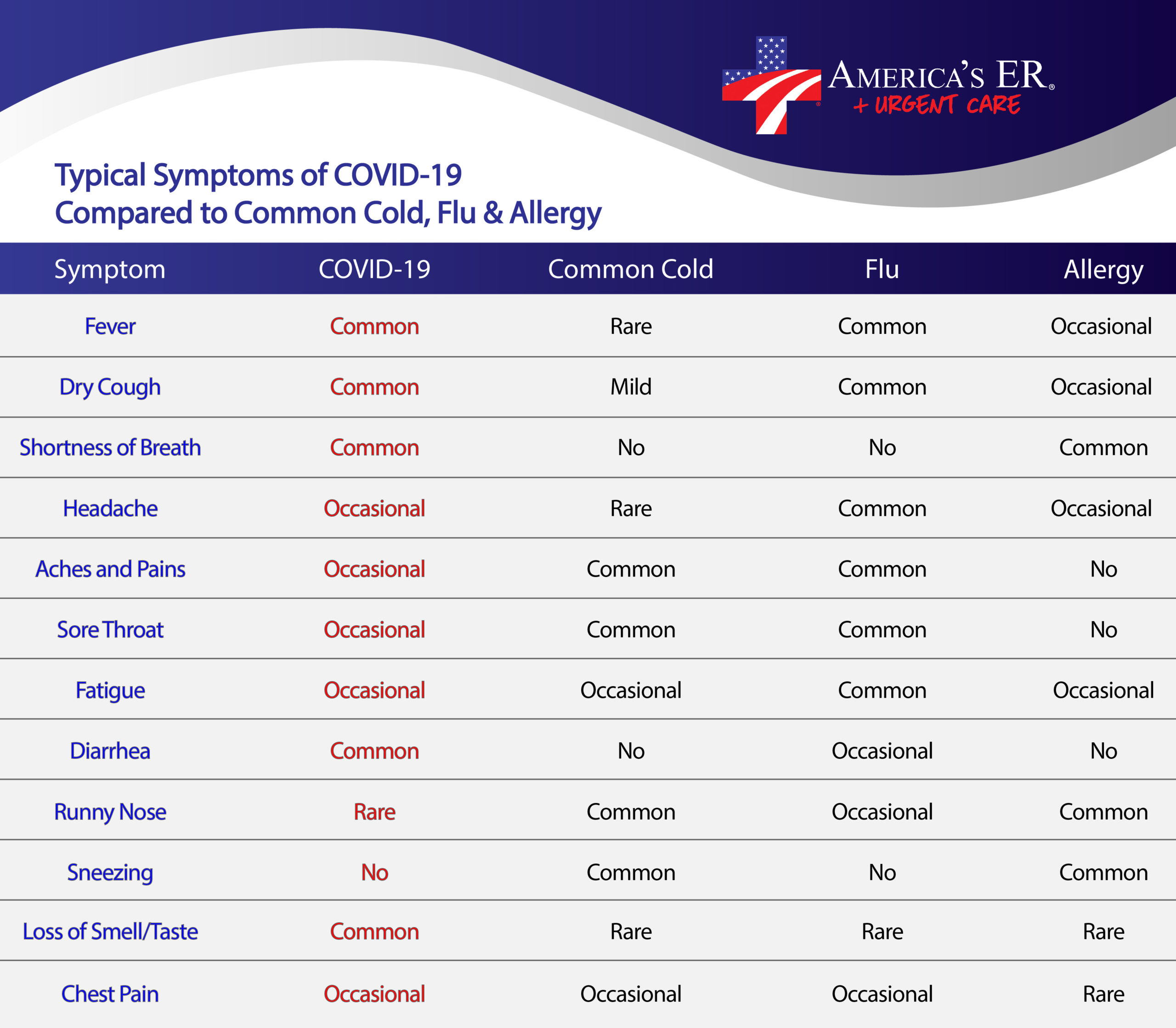
Why am I getting tested for the flu also?
Because the symptoms for the flu and COVID-19 are so similar, the Center for Disease Control (CDC) is now recommending co-testing for influenza (the flu) when testing for COVID-19. At this time, we are co-testing for the flu using the same specimen we use for the rapid-antigen test. No additional swabbing or specimen collection is necessary. You will receive your rapid-flu test results at the same time you receive your rapid-antigen COVID-19 test results.
Do I have to pay for the flu test?
According to the CARES Act and the Family First Coronavirus Response Act, all CDC testing recommendations must be covered by your insurance company with no cost-sharing or other out of pocket expenses to you. That means when you use your insurance, you will not have to pay anything for CDC recommended testing during the national health emergency.
Antibody Blood Test
What is an antibody?
Antibodies are your immune system’s way of remembering how it responded to an infection so it can attack again if exposed to the same pathogen. People with antibodies for a specific virus have a lower risk of infection because their body has already created immune cells to fight it. By looking for these antibodies, specifically IgM and IgG, we can show if someone has already been exposed to a particular virus. IgM, the body’s largest antibody is seen about 7 days after you are infected and typically goes away over the next week or so. IgG, the most common antibody, starts to form when IgM starts going away and indicates you are recovering from the infection. When you are infected by SARS-CoV-2, also known as COVID-19 or coronavirus, your immune system produces IgM and IgG antibodies that are specific to COVID-19. If these specific antibodies are present and there are enough of them in your system to be detected, we have evidence your body has generated an immune response to the virus by producing antibodies to fight the infection. Which of these antibodies are present, if at all, can also tell us where you are in the infection process (early, active infection, recovering, or recovered and possibly immune) or if you may not have been exposed.
What is an antibody blood test and why are they important?
Antibody blood tests, also called serology tests, do not look for the actual virus in your system like a PCR swab test does after you provide a sample from your upper respiratory tract (nose or throat). Instead, this test uses a small amount of blood, typically from a finger stick, to detect if specific COVID-19 IgM and IgG antibodies are present in your system. These tests are important because they can tell us if a person was exposed to COVID-19 regardless if symptoms were present or the infection was asymptomatic.
Click here to read A Case for Broadening both PCR (Molecular) and Antibody Testing of COVID-19
Who should get an antibody test and when should I get it?
Antibody testing should occur after you have had symptoms for at least 7 days, if you tested positive with a PCR swab test a week or more ago (even if you have recovered), or if you were exposed to someone with a confirmed case of COVID-19 at least 7 days before getting antibody tested (regardless of symptoms). The reason for this is to ensure your immune system has had enough time to generate antibodies so we can detect them with testing.
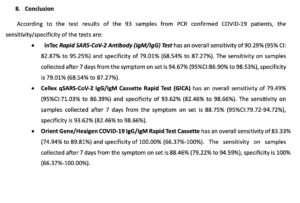
Are they accurate?
Yes. While most antibody tests have not been approved by the FDA, in times of national emergency, many manufactures of these test kits, including those used at our testing facility, have been issued an emergency use authorization (EUA) from the FDA after proving their test kits deliver reliable and consistently accurate results for detecting COVID-19 antibodies. Our test kit, Orient Gene, was approved by the FDA for emergency use as of June 1, 2020 and the next step in the process will be full FDA approval. Read press release here.
Orient Gene has already achieved CE status in Europe and has also been independently tested and verified by the WHO when they compared our test kits to the only FDA-approved antibody point-of-care test made by Cellex. In those studies, Orient Gene outperformed Cellex and others on sensitivity and specificity 7 days from symptom onset.
To further ensure the Orient Gene test kits used at our facility would perform as promised, we conducted our own internal study to confirm their statements. We learned early on in our internal study that these kits, when conducted in the right temperature and humidity-controlled environment (such as in the temporary buildings you see at the testing site), resulted as expected and published. Once our study was complete, we began offering antibody blood testing using these kits to the general public. Please be aware other locations offering this type of testing may not have conducted an internal validation study to confirm their test kit’s accuracy. If you or someone you know has received or plans to receive antibody testing from another location, be sure to inquire if they have validated the accuracy of their test kits and how they did it.
If your test shows you have antibodies, we are confident to say you have likely been exposed to COVID-19. However, no test is perfect and negative results can occur if you have only had the virus for a few days. It is also possible to get exposed and not develop antibodies.
Click the image below to see a summary from the WHO study comparing our test kit (Orient Gene/Healgen) to others. Note that at the time of this study our test kit out performed Cellex (the only FDA approved LFA (lateral flow assy) antibody kit at the time of this study).
Click here to read the product insert for the Orient Gene/Healgen test kit.
Is your antibody test FDA approved?
No. However, the FDA has issued and approved the manufacturer of our antibody blood test kit as an emergency use authorization, or EUA officially on June 1, 2020. Read press release here. An EUA is only issued from the FDA after proving the test kit delivers reliable and consistently accurate results for detecting COVID-19 antibodies. As a part of this strict process, the test kit must go through an application process that requires repeated submission of data and performance of the test kit. As part of the FDA review, a National Institutes of Health (NIH) study comparing rapid test kits found that our antibody test was among the top performers.
To further determine if our test kit would perform as promised, we conducted our own internal study to confirm the manufacturer’s statements. We learned early on in our internal study that these kits, when conducted in the right temperature and humidity-controlled environment (such as in the temporary buildings you see at the testing site), resulted as expected and published.
Click here to read the EUA statement from the test kit manufacturer.
Why do you charge $75 for the antibody test?
The cost of antibody testing includes the test kit itself, staff to collect the test, all of the PPE, equipment, supplies, and infrastructure needed to administer and support testing, your teleconference with our medical providers, and everything else you see at our drive thru testing location. All pricing is based on specific codes used for testing and Medicare rates established by the government. If you have insurance, you will not have any out-of-pocket expenses for testing.
When will I get my results?
The antibody test takes about 15-20 minutes to produce results. You will be called by one of our medical providers the same day that you take your test to go over results. Please note it may take several hours to receive your phone call due to the number of patients our providers are calling but you will receive a phone call the same day of your test.
Will the antibody test tell me if I have COVID-19?
Not exactly. A good way to illustrate this point is to think about when you see damage to an area that was caused by a tornado. Because we all know what tornadoes can do and what the devastation looks like, even if we don’t see the actual tornado, we can make a pretty good assumption that a tornado touched down somewhere nearby and caused all the damage. The presence of antibodies allows a similar assumption. If we see COVID-19 specific antibodies, we can assume you have been exposed sometime in the past to coronavirus because these antibodies wouldn’t be present otherwise. However, because we are not testing for the virus itself and only the body’s response to the virus, these tests are not used to diagnose COVID-19 infections.
Will an antibody test tell me I’m immune to COVID-19?
If you have the COVID-19 IgG antibody, you may have some level of immunity to coronavirus. However, because the virus is so new, experts do not know how long these antibodies might protect you. Some scientists think COVID-19 antibodies provide up to 6 months of protection against future exposure.
Can I go back to work after getting this antibody test?
Antibody tests by themselves cannot confirm if you are cleared to go back to work because it is only half the picture. While antibody tests can show how common COVID-19 is in a population and how much it has spread based on the number of people with COVID-19 antibodies, it doesn’t tell you if you still have the virus in your system. Furthermore, if you are early on in your infection your immune system may not have had enough time to make these antibodies.

What are the symptoms? How does it spread?
Symptoms of COVID-19 are usually fever, cough, body aches, and can include headache or even difficulty breathing. According to the Centers for Disease Control and Prevention (CDC), Coronaviruses in general can be spread through the air by coughing and sneezing and through close personal contact, such as shaking hands. Coronaviruses can also be spread by touching an object or surface with the virus on it and then touching your eyes, mouth or nose.

Who can be tested and how is COVID-19 diagnosed?
Much like testing for the flu, your healthcare provider can order your test and will obtain a swab or sample from your respiratory tract and send that sample to their local department of public health. There, your sample will undergo a test called RT-PCR, an advanced test looking for the genetic code of COVID-19. The CDC will then confirm those results which can take up to 5 days.

How can I protect myself from COVID-19?
The best way to prevent infection from COVID-19 is to avoid being exposed to it. That means staying away from outbreak areas and people who have been infected.
You can also take everyday precautions that help prevent the spread of respiratory illnesses:
- Wash your hands regularly with soap and water for at least 20 seconds. If soap and water are not available, use hand sanitizer that is at least 60% alcohol.
- Wash your hands regularly with soap and water for at least 20 seconds. If soap and water are not available, use hand sanitizer that is at least 60% alcohol.
- Avoid touching your eyes, nose and mouth with unwashed hands.
- Do not come in close contact with people who are sick and stay at home when you are sick.
- Clean and disinfect frequently touched objects and surfaces.
- Cover your cough or sneeze with a tissue, throw it away, and then wash your hands.
Latest from our blog
How Houston Honors Its Military Heroes
Like many cities in the United States, Houston honors its military heroes in various ways.
BUZZ! When Insects Are Deadly
Immediate Actions When Facing Anaphylaxis from an Insect Bite or Sting
Emergency Egg-cellent: Dealing with Egg Health Emergencies
Spring is upon us, a time when many families increase their egg use. With Easter falling on March 31st this year, the eggs will be flying off supermarket shelves. Whether you’re dying Easter eggs, making breakfast, baking a cake, or whipping up a quick dinner, eggs play a significant role. But what happens when your eggs are not as fresh as they should be or you encounter an egg-related emergency?
Putting Our Hearts Into Caring For You
Step into our world, where compassion is not just a word but a way of life. At America’s ER, caring for you goes beyond medical treatment; it’s about putting our hearts into every moment we spend with you. Join us on this journey of compassionate care, where your well-being is at the core of everything we do.
Compassion Drives Our Healthcare Approach
Compassion lies at the heart of healthcare, shaping the way we provide care, connect with patients, and foster healing. It is a fundamental element that goes beyond medical expertise, ensuring that patients are not only treated for their ailments but also cared for on a holistic level.
How To Prepare For The Best Christmas Ski Trip Ever
Planning a Christmas ski trip can be an exhilarating experience, filled with the anticipation of hitting the slopes, enjoying après-ski festivities, and immersing yourself in the magical winter wonderland. However, to ensure a truly unforgettable holiday adventure, proper preparation is key. From selecting the perfect ski resort and gathering essential gear to designing your itinerary and adding festive touches, this article will guide you through the steps necessary to make your Christmas ski trip the best one yet. Get ready to carve through fresh powder, savor hot cocoa by the fire, and create cherished memories that will last a lifetime.